Text: Baroness Julia Neuberger on death and dying

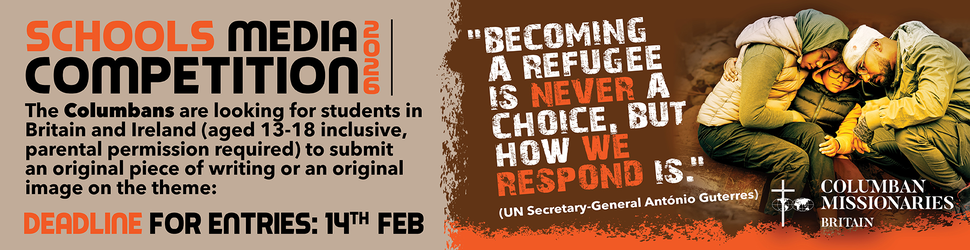
Baroness Julia Neuberger with Catenians Gerald Murphy (left) and Tom Forde (right) who assisted on the evening.
Baroness Julia Neuberger, Senior Rabbi to the West London Synagogue, became the first Jewish religious leader to give the Tyburn Lecture at Tyburn Convent in London, on 23 June.
Speaking on the subject of death and dying, in a gentle and sometimes quietly humourous way, Rabbi Neuberger said the subject was particularly important now, given the political debate on euthanasia and assisted dying and the 'demographic timebomb' society in the West in facing.
She reflected on how we can prepare to die well - choosing where to die, who is to be present, deciding when one wants no further treatment, saying proper goodbyes, and leaving an ethical will. She also looked at how we can support people who are grieving, and asked whether our religious rituals are sufficiently supportive, or whether we could, and should, do more.
Rabbi Neuberger said she felt the Jewish and Catholic faiths had a great deal to learn from each other. She praised the hospice movement and said she felt the Catholic tradition helped people to die better, but she said the Jewish tradition - during which there are special prayers and a bereaved family must stay home or a week while people visit them and bring them food - helps people through the grieving process. "I do think we are better at that because the rituals are more valuable. Seven days being at home - having someone around, however much you get irritated at the end, however much you won't want to see a roast chicken ever again.. is actually is quite helpful.. and then you have 30 days of less mourning during which you go on saying the mourners' prayer every day..."
Baroness Neuberger said she thought it would be helpful for people and make for a happier society in general if people spoke more about death.
The full text follows:
Baroness Neuberger - 11th Tyburn Lecture 23rd June 2011
"Ladies and gentlemen first of all thank you so much for that very generous introduction. Secondly I would like to say a blessing in Hebrew because I gather I am the first rabbi to have given the Tyburn Lecture. I don't know if there are any Jews here but I am going to say the blessing … which is the blessing when something good happens or it is the first time that something has happened. It goes like this …. 'We praise you Lord our God, king of the universe who has kept us alive, kept us going and has allowed us to reach this time'. That is what we say when something is first or new or very good. That this is new, that I am the only the second woman to have given the Tyburn Lecture - may there be many more - I thought it was appropriate. I also think it is appropriate for to say just a few words in Hebrew for people to hear what it sounds like although anybody who speaks Hebrew fluently would say I have got an English accent.
Now, I am going to address issues around dying well and the reason I want to do that is that you have political argument that is going on currently in our society - which is euthanasia versus a huge problem with too many old people and you know this is a demographic time bomb, is what they're telling us, and society doesn't know what to do with its old people and all of that, much of which I have to say I find deeply offensive, I don't know about you. So I want to talk about how we might want to look at pproaching death in a rather different way, and I am not going to talk about euthanasia or about assisted suicide. I am going to talk about preparing to die well and how, as religious communities in the broader community, we can help people to do that well.
I am going to start with a quotation from the Second Book of Kings. 'When God said to King Hezekiah: "Set your house in order for you shall die..." (II Kings 20:1-2), Hezekiah turned his face to the wall and prayed, reminding God of the good things he had done and the things for which he deserved a rethink of the sentence of death. As people will remember from his story on that occasion he recovered and for that he got an extra 15 years of life.
So in my tradition, the Jewish tradition, we are not good at dying. We don't die well.
We've raged and we've stormed. Within the Jewish tradition as a whole, life - chayyim - is the greatest blessing, when we raise a glass, a toast to life. From the earliest rabbinic teachings we've been taught: 'One single man was created in the world, to teach that, if any man has caused a single soul to perish, it is as if he has caused a whole world to perish. If any man saves alive a single person, it is as if he has saved a whole world.' (Mishnah. Sanhedrin 4.5)
In my tradition life is God's gift, and the emphasis is quite clear that we had better value it, and do anything we possibly can to preserve it. So in the Jewish tradition doctors, physicians, are held in the highest regard (which is not always the case in modern British society) - and there are lots of doctors in the Jewish community - and the reason they are held in such high regard is because they are thought to have been given the power to heal by God. So in Ecclesiasticus (Ben Sirach 38:1-2) we find this: 'Honour a physician according to thy need of him, with the honours due unto him. For verily the Lord hath created him.'
So, according to my tradition, the doctors are able to cure and to preserve life. In this line of thought, they become divine creatures beyond ordinary people, because through them life can be preserved. And in our Jewish tradition, we have traditionally put ourselves through everything, all sorts of interventions, even with tiny chances of success. I would often argue that's too much, and we have done that to preserve life. I don't think we have been kind in the process and I would say that the Catholic tradition and from the Catholic tradition the creation of the modern hospice movement and then as it was refined by Dame Cicely Saunders out of the Protestant tradition, I think that that has been a far better approach to death and that's one of the reasons why I thought it was good to talk about this here because I think my tradition has something to offer but I think that Christian tradition has something to offer and it would be really great if we could learn from each other and do it well in both ways. Now I think that's what I'm trying to say.
Medical training has reinforced an attitude that you do absolutely everything to preserve life based on a belief that the doctors' job is to cure and to keep people alive. And that leads to a corollary, which I think has been deeply unkind, where if somebody dies it is regarded as a failure of the doctors and nurses, they didn't try hard enough to keep somebody alive. As most of us die in hospital, with the numbers going up again after a gradual fall for some years, and the assumption therefore must be that we are there because the doctors are still trying to get us cured, to live life. And when we die we - and they - are failures.
Now I come from a tradition where people obviously do view death as a failure and I say, you know, we get old and eventually we die and what matters is what you do in between, but still. There is another piece from my favourite book of Ecclesiasticus which is what doctors should do when he or she sees that the end is near. Listen to this: (Ecclesiasticus Rabba v.6): 'Even when the physician realises that the end is nigh, he should order his patient to eat this and drink that, not eat this and certainly not drink that. On no account should he tell him that the end is nigh.'
Yet actually if we are dying we might want to put our affairs in order, or might want to have a conversation with our family about what comes next. Indeed, I'd argue that we should all be thinking about what we want to happen when the time comes, how we want to die, where and when, and who we want to be there. If we are not told the truth, it is extremely hard to plan.
Even worse in traditional Judaism, in the commentary to our legal code, the Shulchan Aruch, we read: "It is forbidden to cause the dying to pass away quickly; for instance, if a person is dying over a long time and cannot depart, it is forbidden to remove the pillow or cushion from underneath him." And you could find the same in some Muslim codes. And indeed in my tradition we simply don't make the going easy.
There is one wonderful exception, which I love, when the maidservant of Rabbi Judah ha-Nasi, the Judah Prince, the supposed compiler of the Mishnah, one of our earliest codes, had decided that his pain was intolerable and she wanted to stop it. All of his students were surrounding his house and praying for his life to be spared. So she went up to the top of the house with a huge great earthenware jar and she dropped it made a huge noise which meant that they lost attention for at least a couple of minutes, and they were thinking what was all that, with the result that their prayers were interrupted and he slipped away. His suffering was over, and, interestingly, although that is completely against our tradition nowhere in the text does anyone ever condemn her. And a good thing too, you might say!
So why are we so life-affirming? We recognise that ultimately we must surrender to God's will, and that God is just, both also hold a strong belief, and some people think this is a medical tradition and we have inherited it partly from the Greeks, that you must do everything you can and try every medical intervention you possibly can. It may be, and it is worthy saying it here in Tyburn Convent, that Jews are what you call a bit shaky on the afterlife and, since we know what we have in this life, we tend to feel it is as well to stick with it as long as we can. My Orthodox coreligionists assert as an article of faith in their daily morning prayers that they believe in an afterlife, but quite what that afterlife is like is pretty unclear. There are statements by the rabbis of old about all this life being a prelude to the world to come, but they are relatively late, and there's little evidence of earlier traditions in Judaism. The belief which is absolutely clear is in the existence of a place called Sheol, the pit, which you read about in the Old Testament or what we would call the Hebrew Bible, the shady place where nothing much happens and where all is colourless. And, though that does not produce fear amongst Jews, it does seem to produce a determination to hang on to life, whatever it's like, possibly for a bit too long.
And that view of what the afterlife is like goes deep. Many years ago, my father, a very committed Jew, was in hospital and had just emerged from a few days in intensive care. He was being 'specialled' by a lovely young Irish Catholic nurse. I have to say it was just up the road at St Mary's Hospital. They got talking, and it emerged she had been in intensive care a few weeks before my father, after a somewhat terrifying reaction to some kind of an injection. She had been quite convinced she was in heaven - it was shining and white, she could see a cross on the wall opposite, and to cap it all her grandmother was there - so she knew that's where she was. My father meanwhile said it had not been like that at all - it had been grey and shadowy, with shadowy figures flitting about, and dull and soundless.
They talked about it for some time and then laughing, they went over together to intensive care, the nurse pushing my father in a rather grey-greenish wheelchair, and they peered into the intensive care ward. Neither of them was right! It was actually green in colour - with green walls and staff in green gowns flitting about. And it was anything but shady and silent, but it certainly wasn't white or shining either. Each of them had in their deepest psyche a view of what the afterlife was - and they had seen it in intensive care - except it wasn't there.
I tell this story because I think it is important to realise how conditioned we are by our expectations. That's why it is so difficult to change attitudes. If Jews have traditionally been so life affirming, of course they would find it difficult to be enthusiastic about modern ideas about a good death. Yet if you don't be enthusiastic about a good death you are in huge risk of dying in bits, intubated - with lots of bits of piping one way or another - in pain, suffering, and for no purpose. So there has to be a moment where the medical interventions should stop. There is a point where length of days should not be a goal in itself. There is a point where dying well, and going peacefully into that good night, is a goal to be desired.
Now we know from many, many surveys that most people want to die at home, a few people want to die in their gardens, or occasionally on a boat. There is a wonderful Chinese man who wanted to be sure his family had made all the right preparations for his funeral, and insisted on dying with his coffin in the room with him. We found it a bit disturbing at first, but we soon found that it gave him huge comfort, and that people of all backgrounds, of all kinds, like planning their own funerals- and of course most of us do like telling our families what to do!
Christianity has lessons for all of us here. Broadly speaking, Christians are pretty interested in the afterlife, and some people find planning their funerals a way of thinking about what comes next. Other people focus on the actual journey to the hereafter, and for Dame Cicely Saunders, the founder of the modern hospice movement, as we have it now, and for the Sisters of Charity and St Joseph's Hospice before her, it was absolutely clear that the journey to the afterlife should be a good one. If suffering and pain made that impossible, something should be done about it.
Part of Cicely Saunders' revulsion towards people dying in pain and without dignity, was related to her Christian faith. For her, and by extension for the rest of us, the good death was a goal much to be desired.
Some people would say that the fact that the modern hospice movement grew up in Britain is related to the proverbial British 'stiff upper lip', the sense that, whatever the pain, whatever the tragedy, we can't scream or shout. Now I don't think that's right. First of all, it really started in Ireland rather than in Britain because the original hospice was the Hospice of the Sisters of Charity in Dublin.
Secondly, I believe the rootedness in the Christian tradition is much more compelling as an explanation. To journey on well into the afterlife, one needs to have a good death - die well, in fact. And that a good death should let us think about this life, come to terms with what we have and haven't done, sort out any complications or rows with family and friends, and die at peace. And that means sorting out the environment in which we die. And I would argue, and it's from the hospice movement, that people's dying moments should not be clinical, not be in hospital, shouldn't be away from those they love. Ideally, we should die at home, under our own control - experiencing human moments, not mechanical ones. One of the reasons is that it is not just about having a good death and preparing for the afterlife but actually for the people who ill be there after you have gone, the people who are going to grieve for you.
One of the things we know, and we have hard evidence of this, is that if somebody you love has had a good death is that although you grieve for them and although the pain of losing them is huge the pain is assuaged by the feeling that you gave them the best you possibly could and they suffered as little as humanly possible. And therefore it seems to me that there is something we can do for the grief of the people we will leave behind if we ourselves choose to die well and whether that means dying in a hospice or whether that means dying at home or for many of us, alas, dying in hospital it does seem to me there is something important about us dying well in compensation for those we love so that their grief is also assuaged to some extent as well as our own pain and going.
We won't all manage all that. It' is not possible for all of us to have a good death. But I think those goals should be there in government policy and medical practice. It is just as important for our partners and children, our families and friends. I feel better about both my parents' deaths, much as I miss them, because they were both able to die at home, wonderfully cared for by district nurses, palliative care teams, and amazing GPs, all sorts of people. I know I feel better about their deaths because they got what they wanted when the time came - to be at home and simply slip away. I think we know grief at the loss of loved ones is a barren place, but it is gentled if you feel that all that could have been done was done, and that the people you loved had the kind of death they wanted, with whoever they wanted there. We know how to provide a good death when we try. But, all too often, when we fail, we end up with deaths in hospital or nursing homes, unremarked on, failures, in pain and suffering, however hard the staff try to make it otherwise. And there is no benefit to that at all. Suffering is bad for people, so a good death first of all means getting rid of the pain as best we can - and then the real possibility of dying as you want, pain free, thinking emotionally, spiritually, and sometimes practically about what is to happen next- even if you believe it is nothing at all.
Let me give you an example: when my father was dying, he could not quite manage to die, though desperately ill, until he had managed to get back to his own bed, in his own home. He had been in an acute coronary care ward, with end stage heart failure.
We took him out to Regents Park for the day, four days before he died, returning him at teatime on the instructions of a very impressive staff nurse she said that he could 'go at any moment'. But he wouldn't do that. Instead he stayed alive - just - till an ambulance could be organised to take him home after the Bank Holiday - strong advice for everyone here: don't die on a Bank Holiday, it is a very bad idea, it is really inconvenient because the system doesn't work. There he was in hospital on the Tuesday after the Bank Holiday. We took him home and he had a wonderful last day at home, his bed made up by the GP, the district nurse holding him in her arms, his family were all there, he had a lovely Marie Curie nurse looking after him, and as ever the man he was, a book on his knee. He got to see his beloved plants on the balcony, and he knew he was back home. He was a bit like a dying animal, which is what we all are, he wanted to crawl back into his hole. As a dying human being, he wanted us around him, and he wanted to be as free of pain and fear as it was humanly possible to be.
Now I think he had a wonderful death, if you can talk in terms of a wonderful death. But it is only possible for most of us if we happen to be dying of cancer, motor neurone disease or AIDS. For the rest of us unless you are very lucky to live in one of the boroughs where there is palliative care, whatever they are dying of, you actually don't get the chance to die like that and I think one of the things people of all faiths together, one of the things we should do, is to campaign for the right of everybody to get access to services that enable them to die well. It seems to me that It is spiritually important, emotionally important and it is physically important. I think we should do more.
Now, there is something else, which is what we leave behind us. When I was studying to become a rabbi, I became completely fascinated by ethical wills, a sort of like a last will and testament where you leave your possessions except that it isn't your possessions, where you leave a letter basically saying to your nearest and dearest what was most important to you in your life. They weren't about money, possessions, property, and dividing things up. They were the last moral will and testament of teachers and sages- and they made for fine, if sometimes eccentric, reading. They did things like telling their children when to read particular religious books, and when to think about getting married. They told them to look after their mothers and their sisters. They told them to beware dishonest traders and always to give the benefit of the doubt to somebody who comes begging. And they tried to sketch out what a good life might be. It is a lovely custom, with parents trying to sum up all that they had learned in life in a letter to their children, in which they would try to express what they wanted most for their children. These letters were left as a precious legacy because the parents believed that the wisdom they had acquired was just as much a part of the legacy they wanted to leave their children as any material possessions they happened to have.
I really found that interesting and I started puzzling around whether we could do something with it and turn it to more modern use, if you like. I got talking to a friend who is a hospice nurse and a Catholic. I started reading a typical ethical will which made me laugh a lot. It was all about a rabbi trying to persuade his congregation to cease gabbing, to gossip less, and kept talking about how pretty offended he was by women talking like frogs. It was deeply offensive but you know full of stuff like that. I was talking about it as a tradition and she said it reminded her of what a lot of young women do who were dying, particularly when they are dying of breast cancer and were of a young age with small children. Very often they didn't leave a letter, some do, but most leave a box but some leave a box of treasured possessions for their children, because children of course wouldn't remember them very often and they put these boxes together and they put favourite bits of fabric in and charms and bits of jewellery, just sentimental things that meant something to them, sometimes books, a little letter saying how much their children meant to them, how they were the apples of their eye. It does seem to me that that is a really important thing to do and we don't do nearly enough of.
Thd tradition of ethical wills and leaving something for the people who come after us is something we can learn a lot from.
Now clearly these boxes are not the same as ethical wills. They are simply a letter but there is a real similarity of purpose here and I do think it is worth us leaving a letter to our descendants or friends whoever they may be, saying these are the things that mattered to me, you might want to think about them, and by the way I really loved to have known you and really loved having been close to you and all of those thoughts. One of the reasons for doing that is I think it gives us something to focus on as we near the end. The other reason is that it is hugely comforting to the people who receive them. It is a way of helping people to grieve better. It is a way of saying to the people who are going to have lost you, 'actually I am gone but some of the things that matter to me can matter to you, some of the things that I was about can be some of the things that you are about too. I think that there is a really important lesson for us there. It is a tradition that is largely gone but is beginning to be reinvented in the States and that is about how we face up to our own deaths, prepare what we want to say to other people and to write after that in some way … other people would find comforting when the time comes.
Some people would say it is just a last ditch attempt for parents beyond the grave to control their children, it is a bit like people saying you can't have any money until you are 43. But if you craft it in the right way it isn't about money or control of one's children, it's about saying 'here's something I minded about, you might mind about'.
So I think there is a lot we can do to change the way we face death and change the way in which we encourage people to grieve.
I would like to say something else about grief. I have already said to you that I think Jews are pretty bad at dying. We are really pretty good as people who grieve and we have rituals that are enormously beneficial. Funerals take place very quickly, as it does in the Catholic tradition in Ireland, and then there is deep mourning for seven days and the community and people are expected to come to the house of mourning and to be there and offer sympathy and bringing food and have evening prayers with the family of the people who are bereaved. And it goes on for a week. Having been through it twice in my life there is a point at the end of the week where you are so glad to see the back of them. You have really had enough. You haven't been left alone for seven days. But, you know what, it allows you to get beyond the first stage of grieving and you get to a second stage where you can start slightly to face outward. And you know that 300 or 400 people have helped you to do that and the community has helped you do that.
In the Christian tradition there was the thing of having prayers on the third and sixth and ninth days after death. As Christians have taught Jews to die better I think we Jews can teach Christians howto grieve better and I do think we are better at it because the rituals are more valuable - seven days being at home having someone around, however much you get irritated at the end, however much you won't want to see a roast chicken ever again, but that actually is quite helpful and then you have 30 days of less mournful and you go and say the mourners' prayer every day.
I think it is quite valuable. It is quite a trial for people. It is quite a discipline but I think it helps them grieve. I also think it puts the obligation on the community to help them grieve. People have to say Kaddish, there has to be a group to do that. In Orthodox Judaism there has to be 10 men present, in my tradition 10 male or female people. But you do need community to say Kaddish. I think the community is then bound in to helping people grieve and I think there is a tradition in that which you take much wider society to helping people grieve. I think bereavement counsellors do a great job but actually we should be using bereavement counsellors for abnormal grief when thing are strange or have gone really wrong. For most of us our friends and family and community should be there as support when we are grieving and we should have rituals that make that possible.
I would like to say something about the sharp end. I was involved, as were many people here were indirectly, in what used to be Age Concern and the Millennium Debate of the Age and I chaired the group that looked at health and social care and we spent enormous time putting together a charter of what one should be able to expect if one is dying and what sort of choices one should be able to make.
We are going to go through the euthanasia debate again, I am sure we are. We are going to go through the physician-assisted suicide debate again, I am sure we are.
Just so everyone knows, let's be very clear, I am not in favour of euthanasia, I am not in favour of physician-assisted suicide. I don't think it is a good idea for our health professionals to kill their patients any more than they do accidentally, I just don't think it is a good idea.
I do have some sympathy - and many people I think will disagree with me - I do have some sympathy with the idea that that people who are already terminally ill and finding their situation unbearable, that they should be given the wherewithal to take their own lives. I am sure that many people - those who are true Catholics will strongly disapprove of that and there are Jews who strongly disapprove of that - but I do have some sympathy because there are some people for whom actually life becomes unbearable when they can't control the pain. I think it is the exception. All the experience where that has been tried, for instance, in Washington State in the United States has shown that when people are given the wherewithal they barely ever use it, which suggests they want the reassurance rather than the actual capacity to deal with it.
I absolutely disapprove, in any way whatsoever, of health professionals killing their patients, although sometimes they do by accident, but that's another matter.
This debate is going to run and run. We are not going to get away from it in any way in our lifetimes. My guess is that at some point there is going to be a change in public policy because if you look at the huge range of public opinion you will see that young people are more in favour of people being able to take their own lives or indeed to ask health professionals to do it for them. So I think we have a battle on our hands.
If all that could be left to one side, what are the things that we most want to say about how we want to die? This is what a whole group of us, working for many hours over many days came up with. First of all you might like to define what a good death might be like and I think some of us might recognise a good death when we saw one but need not agree on a definition. That's why Age Concern came up with its definition. If we could define what a good death might be then you might be able to say what people ought to access if they could.
I do think that the religious people should be pushing for that. I have to say by the way that it took some doing. The British Geriatric Association signed up to these as principles and health professionals are increasingly signing up to this, which should see some improvement. We first of all thought - many people might wish to disagree - I think we should be able to know when death is coming so we can decide what might happen to us in the very end stages of our lives. So we need to know about that. We need to know about difficulty in breathing, we need to know as much as possible about how we are likely to feel.
Secondly, I think where it is possible we ought to be able to retain control over what will happen. We ought to be able to decide whether we want more pain relief or not. People may know that increasingly in hospices now people are given control over syringes so people can press a button to get a bit more morphine … they control how much morphine they use. Some but not all of the evidence suggests that if you control how much pain relief you are using yourself actually you use less pain relief because 'it is a long wait before the next one'. If you can, some give a little bit of a press and take a bit more you probably in the end use less. The jury is out on that a bit but having control, feeling you can make the decision about how much you use is enormously important.
The thirdly, being afforded dignity and privacy, with everything we have been seeing about what has happened with old people in our hospitals, in our care homes, some of the stuff people have been seeing in the Care Quality Commission, some of the stuff we have heard about from the Equality and Human Rights Commission this week, that's hugely important. It should apply to all of us at some stage in our lives but when we are dying the last thing that should happen to us is that we should be left on a trolley in a hospital corridor with loads of people walking past all the time and left to get on with it.
Fourthly, have control of the pain relief and other symptoms. I have talked a little bit about that but that's also about saying 'actually I don't want pain control'. One of the things many Buddhists say is that they don't want pain control because it doesn't leave them as clear-thinking as they wish to be when they face the end.
I think that the other thing that we have to recognise is that not everybody is just like us. Some people may choose not to have pain relief for other reasons.
Have choice or control over where death occurs. Most people still get shunted into hospital when they are coming towards their end. It tends not to be the best place to die but more of us are dying in hospitals than we were 10 years ago. I think that it is really important that people are helped to die at home, in hospices or wherever they choose. If they want to die in a hospital, well then fine, but if you can be sure that they are able to die at home … then I think that's really important.
Have access to any spiritual or emotional support required. As many people will know, chaplaincies in hospitals leave much to be desired. There just isn't enough of it and most hospital chaplains will spend more of their time comforting and supporting staff than their patients. There is a huge issue about how people from religious communities should and could spend time with people who are dying, be it in hospices, be it in their own homes. There is far more that we could actually do to help people have both spiritual and emotional support.
Then have access to hospice care in any location. Then have control of who is present and who shares the end. Now, as a pastoral rabbi, I have had quite a lot of experience of being with people when they actually approach their end. There is an all too familiar and really dark business of the family already fighting over their possessions …it is deeply unattractive and not wholly uncommon. I think that people who are dying, who are able to tell us, should be asked who they want to be there and do think that you should be able to say to family members who will be difficult 'if that's what you are going to do then, you know what, you shouldn't be there'. I think it is difficult for us to do but I suppose it is right and I think it is one of those things that we could, as religious people actually often supporting dying at home or hospice, can help that happen.
I now think there is something about advance directives. People will have their own different view on that. I think it is important that you are able to write a document which is legally enforceable and says 'in these circumstances I do not wish to have further invasive treatment. That is particularly common these days as cancer has increasingly become a chronic condition rather than an acute condition.
People can be treated for cancer for more than 30 years but many people say they come to a point where they simply don't want any more of the chemical whatever it is. I do think we ought to be able to say whether we want treatment to cease. That is a very different thing from saying we want our doctors to kill us. But I have to say that many people in my Jewish tradition don't approve because they still believe that everything should be done that could be done.
And then the last thing is being given time to say goodbye and having some control over some of the aspects of timing and that may seem rather strange to some people but for many of us the period coming up to our death is probably to be in weeks rather than days or hours. We do know, if we are told, we do know and I think being given the chance of telling people you know, not a few days away, you might want to say your goodbyes and calling people in … I at least think that a lot of people who are dying say they want to make their peace with people they have loved or sometimes hated. They want to sort their lives and I think that it is very, very important that we make that possible and again I think that is something that religious communities can help to do.
So those, if you like, are the things that … have been increasingly taken on board by five health professions. But there are some other things that people who are dying say they want. Here are some of the things, and I haven't got time to go into detail, but it is important. A lot of people say they want quiet time, time to contemplate, time to think, time to pray, time to make it spiritual. A lot of people say they want pain relief, well obviously so. A lot of people say they want to play football. Now, I have always found this a bit strange but I remember one of my first visits ever to St Christopher's Hospice in Sydenham seeing a sort of football match going on between two hospice patients in the corridor. One of the things, particularly for younger men who are dying, is that it is an important part of their lives and they want to carry it on.
I think that for many people who are dying and who have accepted it and who are dealing with it and preparing for it nevertheless they want to do some of their usual things. There will be singing for others, it could be playing football, it could be going to music. A lot of people like going to concerts, it could be a rock concert, it could be an opera or a classical concert but people really do that.
And that other thing that people say that they really want to do is eat things they most like. Now when people are dying at the very, very end of life people often stop eating and that is one of the things that indicates that they are coming very, very close to the end. However, very often for the last few days people get a sudden burst of appetite, and hospices will tell you this, and people want the food they most like eating, and hospices aren't great for providing certain items or providing this sort of food.
When my mother was dying - I remember she died four days after her 86th birthday, she was absolutely determined to have her birthday. My mother was a refugee from Nazi Germany. She came to Britain, she discovered tea and whisky and never looked back. She hadn't eaten much for the previous two weeks but as she came towards her death on her birthday and the day after she insisted on her favourite things. So she had a large quantity of tea, with lots of milk. She liked asparagus, she liked pizza and she like whisky. Here was this woman, who was a very large woman down to about five stone, tucking into an enormous plate of pizza and asparagus, knocking back the whisky and the tea.
This sounds extraordinary but it isn't uncommon and what I think is very important is that you listen to what people who are dying say and if they say what they want is a large whisky or if they say what they want is a plate of asparagus well damn it why shouldn't they have it? Give it to them. Even if they are likely to choke, who cares, they're dying. I think it is really important that we listen to that and take it seriously.
I should probably say that most hospices, but not all, do take round the drinks tray at six o'clock in the evening. If you are in a hospice you are lucky, you will be offered a stiff whisky anyway but that's another point.
So what do we have to think about? I think we have to think about whether we can help people to die well, whether we can face up to dying well ourselves and whether, in the way that we die, we can help people to grieve better. I think if we could do that this would be a healthy society and it feels happier about talking about death, dying and bereavement. At the moment I don't think we have a very healthy conversation and one reason I have chosen this as my subject is that I hope it might encourage you to do a bit more talking about it.
Thank you very much."